
Too often, misconceptions and misunderstandings keep people from reaching out to their healthcare providers regarding palliative care when the truth is that there are many benefits and quality of live improvements to be gained from palliative care. Palliative care specialist Dr. Yee Choon Meng talks about the facts about palliative care, and dispels some of the common myths surrounding it.
Fact: Patients can receive palliative care at any stage of a serious illness. The goal of palliative care is to provide an extra layer of support and increase patients’ comfort by addressing their physical, social, emotional, and spiritual needs. Palliative care should therefore start early in the course of illness; to reduce symptoms and suffering from the beginning, and thereby enable patients have the best possible quality of life for the longest amount of time.
Fact: Palliative care can help people with virtually any serious condition, at any stage of illness, including terminal cancer. For example, palliative care is for people with kidney, liver, lung and heart disease, dementia, multiple sclerosis, advanced Parkinson’s disease, and motor neuron disease, among many others. People of any age, including children, can receive palliative care. In Singapore, there are special Palliative Home Care programs; care for patient with Advanced Dementia (Program DIGNITY by Dover Park Hospice Home Care), end stage organ disease and frailty (Program IMPACT [Integrated Management & PAlliative Care for the Terminally ill Non-Cancer Patients]) and Paediatric Palliative Care patients (Star PALS [Paediactric Advanced Life Support])
Fact: Patients receiving palliative care can also receive other types of treatment for their illness. In other words, palliative care is given alongside treatments intended to cure, control, or modify the person’s serious illness. The primary physician will often continue to see patients in the outpatient settings and collaborate with the Palliative Care Physician in the acute hospital or community (home care or day care) on other aspects of care such as: symptom management, discussion advance care planning, other care plans.

Fact: Palliative care does not hasten death and neither does it prolong the process of dying. Most importantly, Palliative Care does not only look into the symptom management of patients, it also addresses the psycho-emotional needs of patients and their family during this challenging period. In a large randomised controlled trial, patients with advanced lung cancer referred for early palliative care intervention led to significant improvements in both quality of life and mood (Temel et al, New England Journal of Medicine, 2010)
Fact: Palliative care in Singapore is provided in multiple settings. This includes the hospital (inpatient service during admission or outpatient clinic service), hospice home care service provided by multiple service providers, hospice day care services (for patients who are able to engage in activities and be cared for in the day time) and inpatient hospice (for patients who are terminally ill with prognosis that is less than three months and care needs are high). Please refer to the Singapore Hospice Council Website for more information.
There are Palliative Care services provided by Palliative Care physicians in private hospitals and private home care services like Vickycares.
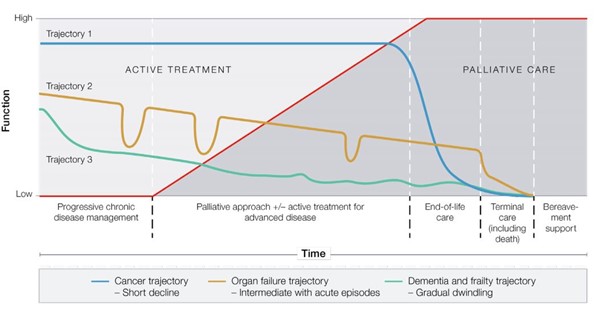
Fact: Palliative caregivers usually collaborates with the primary physician to maintain quality of life, navigate the healthcare system, and explore treatment options. It is a type of care that provides the best possible quality of life throughout the course of your illness. When the life-limiting illnesses progress or the patient is no longer receiving curative treatment, the Palliative Care team will continue to provide care with the goals of ensuring physical comfort, psycho-emotional and spiritual coping for both patients and their family. During this period, the involvement of Palliative Care will increase, while life-prolonging treatments are no longer helpful (please refer to Figure 1). Bereavement follow up are provided for the family with potential grief issues.
Fact: Pain is one of the more common symptoms seen in palliative care. But, patient with life-limiting illnesses may also experience other common symptoms, such as nausea, vomiting, shortness of breath, anxiety, depression, restlessness, spiritual distress, constipation, diarrhoea, loss of appetite, swelling, itching, insomnia, and other issues that may affect the patient’s and family’s quality of life. Hence, Palliative Medicine usually addresses these issues through frequent multi-disciplinary discussion.
Fact: Costs are kept affordable through various subsidies and financial schemes. Government subsidy is available through means-testing for service providers receiving subvention from the government. The level of subsidy is determined by the household monthly income per person. In addition, Medisave can also be used for palliative care services.